You are here
Content
Sandra and Sascha Jonas would like to have a baby. However, they are both obese – which increases the chance of complications during pregnancy. Before their joint gastric bypass surgery at Mannheim University Hospital, they talk about their expectations in an interview.
Obesity Consultation Hour
Phone +49 (0)621/383-2209
(Video consultation possible)
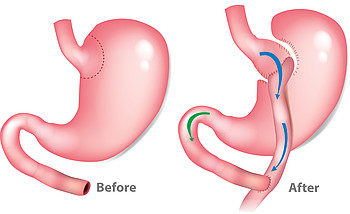
How does the Roux-en-Y gastric bypass work?
The surgery is laparoscopic (using the keyhole technique) and involves making a total of five small incisions in the upper abdomen. The surgery has two aims: to reduce the size of the stomach and to change the passage of food. First of all, the stomach is divided. This creates a ‘gastric pouch’, which is the part of the stomach that remains for the food to pass through. The rest of the stomach is excluded from food passage, but remains in the abdomen. Removing this part of the stomach would increase the surgery’s risk unnecessarily. The gastric pouch is now connected directly to the small intestine and, after about 150 centimetres, the upper part of the small intestine is connected to this part of the intestine again. The rest of the stomach and the first 60 centimetres of the small intestine are therefore excluded from the passage of food. Digestive enzymes are added to the intestine by the pancreas, along with bile in the duodenum, and only come into contact with food at the junction between the small and large intestines.
Changes caused by the Roux-en-Y gastric bypass
Since the volume of the stomach is reduced, the patient can only eat smaller amounts of food to begin with; nutrient absorption is also reduced due to the change in food passage. But, at the same time, this also reduces absorption of vitamins and vital trace elements, so additional intake is absolutely critical. As with gastric sleeve surgery, most patients can eat children’s / elderly people’s portion sizes again after about two years.
A lifetime of care following a gastric bypass
The specialists at Mannheim University Hospital provide patients who have had gastric bypass surgery with post-operative advice and care for the rest of their lives. Potential (side) effects of the surgery: Heartburn (reflux) is extremely rare following this surgery. In many patients, the surgery even significantly improves pre-existing heartburn. If the stomach is not operated on, the pylorus (sphincter at the pyloric orifice) regulates the continuous release of the food pulp into the duodenum. Following gastric bypass surgery, this sphincter no longer exists, or only exists in the part of the stomach that has been eliminated. So the food pulp is passed on to the small intestine very quickly after ingestion. This can result in dumping syndrome, which manifests itself in nausea, dizziness and feelings of discomfort after eating. In severe cases, it can even lead to circulatory problems. Dumping syndrome can usually be managed well by changing diet. The surgical therapy only needs to be repeated in a very small number of cases. An ‘internal hernia’, which occurs in about four out of 100 patients, is another specific complication of this surgery. Both the severing and the reconnection of the intestine creates two gaps between the loops of small intestine, into which other loops of intestine can get squeezed.. The bariatric surgeons close these gaps during the surgery with a suture. However, they cannot be closed completely because they get bigger following surgery due to weight loss. If intestinal loops get stuck in these gaps, symptoms such as abdominal pain, nausea and vomiting can occur. If you experience complaints such as these, following surgery, the specialists at Mannheim University Hospital will discuss the necessary procedure with you in detail so they can determine an individual approach together with you.
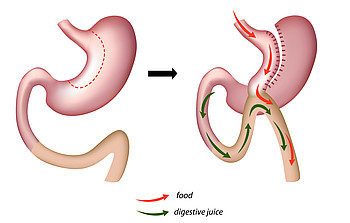
How does the OMEGA LOOP gastric bypass (mini bypass) work?
The surgery is laparoscopic (using the keyhole technique) and involves making a total of five small incisions in the upper abdomen. In this procedure, the left part of the stomach is cut off along the entire length of the stomach first of all, leaving the stomach in a tube shape. Then, part of the small intestine is formed into a loop, guided upwards and connected to the tube-shaped stomach. This bypasses the upper part of the intestine (normally about 120–180 centimetres of the small intestine). Digestive juices from the separated part of the stomach can still pass into the intestine at the same time.
Changes due to the omega loop bypass
On the one hand, the volume of the stomach is reduced and, on the other, the absorption of food is reduced because the first 120–180 centimetres of the small intestine are eliminated from the food passage. This results in good weight loss. But, at the same time, this also reduces absorption of vitamins and vital trace elements, so taking them is absolutely critical. Another side effect of the surgery can be backflow of bile and other digestive juices into the rest of the stomach. This can cause chronic inflammation of the stomach. Since this surgery is not performed as frequently as gastric sleeve surgery or the Roux-en-Y bypass, the after-effects with regard to bile reflux 20–30 years after the operation cannot be adequately assessed yet. One advantage of the surgery is that only one connection from the stomach to the intestine needs to be made; no further intestinal connections are necessary. This makes the surgery easier from a technical standpoint. It is also feasible if the Roux-en-Y bypass is technically not possible.
How does the single-anastomosis duodeno-ileal (SADI) bypass work?
With SADI surgery, a gastric sleeve is formed first of all, then connected to a loop of small intestine. This excludes part of the intestine from the passage of food. The reduction in the size of the stomach and the fact that food bypasses the first section of the small intestine cause a reduction in food intake and the absorption of nutrients in the intestine, as well as a change to the patient’s metabolism.
SADI surgery with a DaVinci surgical robot
SADI surgery is an exclusively laparoscopic procedure performed by a few experienced surgeons. They use the DaVinci surgical robot at Mannheim University Hospital.
As with the other gastric bypass methods, patients need to take vitamins and trace elements for life following SADI surgery. The interdisciplinary team of specialists at Mannheim University Hospital provide lifelong follow-up care and check the blood values at regular intervals. Since SADI surgery is a relatively new procedure, there is no long-term data available concerning the effects. However, initial experience shows that, with SADI, ‘dumping syndrome’ and heartburn occur far less frequently following surgery. SADI surgery increases the risk of swelling of the gallbladder and the development of gallstones. The attending doctors at Mannheim University Hospital conscientiously provide information about other potential side effects.
Context Column
Consultation hours and appointments
Phone +49 (0)621/383-2209
(Video consultation possible)
The obesity clinic team


Dr. med. Georgi Vassilev
Deputy Head of the Rhine Neckar Obesity Centre
Coordinator of the Colon Cancer Centre
Chief Physician of the Surgical Clinic



